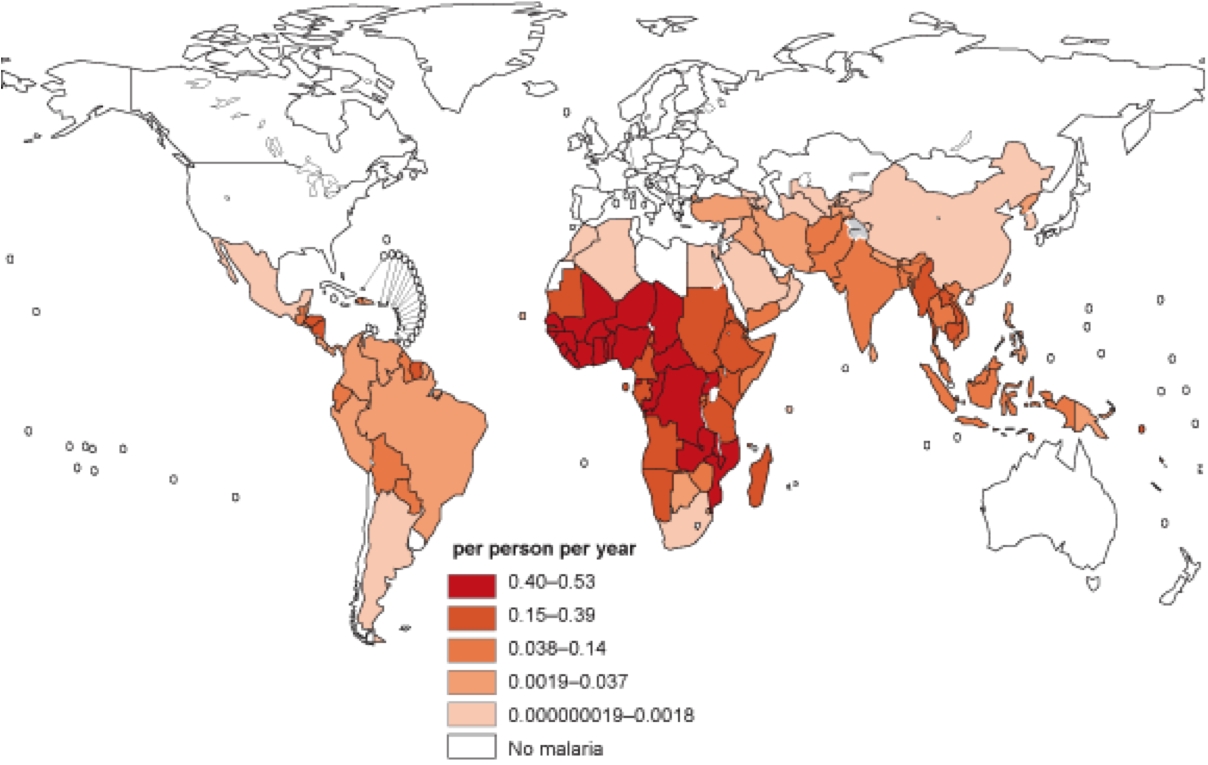
For those on the frontline of the battle against malaria, news of the development of a vaccine against the parasite is an exciting development. In 2013, the disease was responsible for 584,000 deaths, nearly 90% of them in Sub-Saharan Africa; some 78% of its victims are children under the age of five. In the 97 countries in which malaria is endemic, it ravages the economic productivity of those who can least afford it: poor people with limited access to treatment and care.
In July, the European Medicines Agency approved RTS,S – a vaccine also known by its trade name, Mosquirix – for use in children from six weeks to 17 months old. The global health community has long appreciated the importance of a vaccine in reducing the disease’s burden, and the World Health Organization is expected to make an announcement in November about the use of Mosquirix in countries where malaria is endemic, some 30 excruciating years after researchers at the pharmaceutical company GlaxoSmithKline (GSK) began working on the vaccine.
The approval is a significant step in the right direction for the prevention and control of malaria. It is also a testament to the enduring power of social philanthropy, partnerships, and international collaborations. However, many questions about the vaccine’s deployment – and its integration into the health systems of some of the world’s poorest countries – remain to be answered.
Cost is probably the most important issue. Many of the people who most need the new vaccine are poor. It remains to be seen whether “equity pricing” will be feasible, considering the millions of dollars invested into research and development. GSK has said that Mosquirix will be offered “not for profit”; but the pharmaceutical company still must break even.
And who will actually pay? Many African governments have shown some willingness to invest in public health infrastructure in the past; but a political commitment to the vaccine could mean redirection of resources from other important tools, including rapid test kits, cheap drugs, safe insecticides, and long-lasting insecticidal bed nets.
International non-governmental organizations and private foundations have collaborated with the public sector in the fight against malaria, providing funds and bringing attention to the issue. It might be asking too much to expect them to pay for the vaccine.
There are also questions about some countries’ capacity to distribute the vaccine, as well as uncertainty about how it will hold up under real-world conditions. For example, the testing for Mosquirix did not account for the possibility that parents would neglect to use insecticide-treated nets for their children because of a false sense of safety and security provided by the vaccine.
Moreover, in order to maintain the vaccine’s efficacy, a booster needs to be delivered after the initial three doses. Without it, effectiveness drops to non-protective levels. Will governments really be willing to spend millions of dollars on this?
Finally, many parents in Sub-Saharan Africa currently do not immunize their children for a variety of reasons, including distrust of health officials and ignorance. The polio vaccine faced an uphill battle in Nigeria, and the new malaria vaccine could suffer a similar fate. Governments will have to decide whether to make its use compulsory or provide incentives for those who choose to vaccinate their children.
The approval of Mosquirix opens a promising new phase in the fight against malaria. But serious challenges abound. To meet them, African countries must initiate, develop, and support homegrown research capacity and leaner models for delivering care. Research and investment in physical and social infrastructure must be a high priority as well.
In the time it has taken to read this article, five children will have died from malaria. Ten years from now, that statistic could be no more than a bad memory, thanks to Mosquirix. At the very least, the world now has a new weapon in the fight to reduce the disease’s toll.
Credit: project-syndicate.org