Introduction
In order to improve healthcare, most nations embark on the provision of health facilities, training of health personnel and the acquisition of essential drugs. All other things being equal, the availability as well as the quality of these facilities and services ultimately determines the quality of health in a nation.
Health care spending is therefore very critical in every effort aimed at improving the health status of every nation. The desire to achieve universal health coverage (UHC) is a noble one, but it is argued that this objective in particular lacks operational content within the economic context of scarcity and the necessity for choice among equally desirable objectives outside the health sector (Vogel cited in Muazu 2013).
Adequate and efficient health related spending is widely considered as inevitable in the improvement of health outcomes. At the macro level, investment in health workforce and infrastructure is expected to improve health conditions and hence human capital of the population. This article will look briefly at the trends in policy and expenditure towards achieving improved health outcomes.
Facts
The health expenditure as a percentage of total GDP was 5.11% in 2009, 5.29% in 2010, 5.27% in 2011 and 5.17% in 2012.
Public health expenditure which consists of recurrent and capital spending from the government, external borrowings, grants and social health insurance funds was 57.77% of the total health expenditure in 2009. In 2010 public health expenditure slightly increased to 58.51% of the total health expenditure. In 2011 and 2012, the public health expenditure was 55.87% and 57.12% of the total health expenditure respectively.
From 2009 to 2012, the years under review, expenditure allocated for health sector development averaged GHS1.4billion per annum (Budgets Statement, 2010-2013). Given this expenditure and the competing alternatives, one would expect efficient execution of the budget and gradual improvement in the health delivery in Ghana. Far from it! Out Patient Department (OPD) per capita is still low. For the years under review, NHIS funds were not delivered on time and 60.7 percent of insured clients patronized the scheme. Again, the health conditions of Ghanaians as proxied by the health outcomes measured by the MDG targets are far below expectation. As of 2013 the maternal mortality ratio in Ghana was 380 deaths per 100,000 live births as against the goal of 185 deaths per 100,000 live births with a 2015 deadline. Under-five mortality is 78.4 deaths per 1000 births as against the target of 41 deaths per 1000 births.
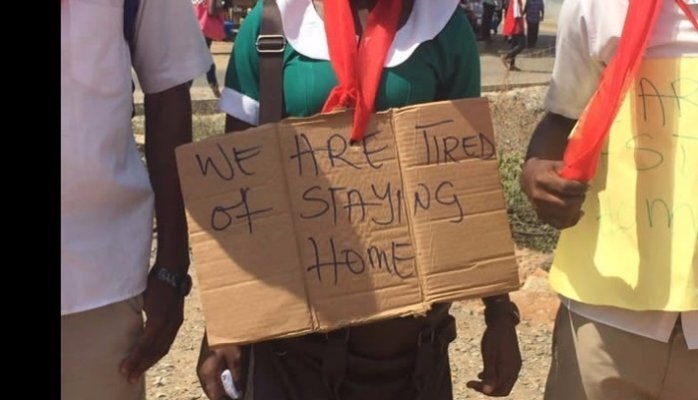
On 11 April 2012, the Ministry of Health notified WHO of a cholera outbreak in the Greater Accra Region. Between January and 6 May 2012, a total of 3,216 cases and 28 deaths were reported from 20 districts. (WHO, 26 May 2012) The cholera cases and deaths increased steadily with the Ghana Health Service reporting 6,000 cholera cases with 69 deaths by the end of August (IFRC, 4 Jan 2013). For the year 2012 as a whole, WHO reported 9,548 cases and 100 deaths (WHO, 7 Feb 2013). This has serious implication for the human capital endowment of the nation and also loss in work days which is a basic measure of productivity. The budget statement reveal a greater percentage of the health expenditure on compensations (88.35% in 2009, 95.21% in 2010, 94.89% in 2011 and 92.27% in 2012), nonetheless the nation has been plagued with episodes of strikes by health workers. The expenditure on service and investment which is actually needed for improvement in health outcomes are very minimal (sum of the expenditure allocation on services and investments for the years under review, 3.83% in 2009, 3.07% in 2010, 4.26% in 2011 and 7.73 in 2012).
On the NHIS, (whose principal aim is to reduce the high dependency on out-of-pocket (OOP) payments in the form of user charges and co-payments, which are regressive as they disproportionately, affect the poorest in society, and therefore challenge the underlying tenets of equity within healthcare systems) active membership of the scheme stood at 34% short of the target of 45% as of December 2012. The National Health Insurance Authority (NHIA) accessed only 48% of all receivable funds during 2012 and this had implication for timely reimbursement to providers. An analysis by the NHIA showed that the scheme cannot be sustained at the current level of operation.
The principle of “paying our quota so we receive the services due us” does not really come to play in the health sector. What the numbers and paper speak (in terms of policy and expenditure allocation) is very different from “what is“. The trend in expenditure does not sync with the expected outcome in health as such, the cheapest way to navigate the current healthcare system will be not to use it. To help curb runaway healthcare spending, policy makers should focus on increasing preventative care i.e. look at whether the more intensive treatments yield improvements in morbidity and mortality? While you can’t prevent everything, taking care of yourself before problems arise is the easiest way to save big. Improvements in health outcomes cannot be attributed solely to the efforts of the healthcare system as health production theory indicates that other factors influencing health outcomes include environment, lifestyle and human biology. Hence the needs for massive education on preventive health care rather than the attention on the curative which is somewhat insufficient.
Conclusion
Ghana’s success story is encouraging but has to be relieved by the high number of exemptions through taxation (as cost to the government of exempting one poor individual from premiums is between US$15.87 to US$95.44) and the threat of moral hazard. In addition to its rapid increase in membership, equity in access in the NHIS can be enhanced through clearly-defined exempted groups that are funded from general taxation i.e. include the need to identify and promote membership for the rural poor. One of the recommended ways is to ensure co-payments especially among the pro-rich and the pro-urban membership in order to dampen demand and partly control costs. This will also help make minimal the problem of moral hazard which drains the scheme.
Source:Imani Centre for Policy and Education